Injuries to the shoulder can generally be classified into 3 groups: Rotator Cuff, Instability and Frozen Shoulder. The physiotherapists treat a lot of difficult shoulders, the most common being Rotator Cuff or muscle imbalance problems around the shoulder. As the shoulder is a very muscular joint, if these muscles are not working properly it can create imbalances and shoulder stresses. Physiotherapy works at balancing out tight or under-working muscles to balance this load. Our shoulders have nearly 360 degrees of range so there are a lot of muscles and soft tissues involved. If the joints around the shoulder are not working, this will also load up the shoulder. Postural issues often cause shoulder pain.
MORE DETAILED INFORMATION:
The diagnosis of a ‘problem shoulder’ can be a complex issue. It is a complicated joint with minimal bony support, which enables a huge range of movement. This leads to problems as, in essence, the shoulder joint is controlled by soft tissue. In other words, a dynamic active joint with the potential to become unstable is connected to an already complicated shoulder girdle, made up of the acromioclavicular joint, sternoclavicular joint, cervical spine and the very important scapulae.
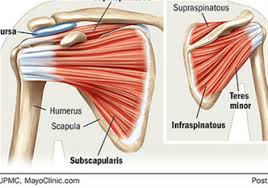
The glenohumeral joint has often been described as a watermelon on a saucer. This is not far from the truth. The socket is very shallow and if not supported by the rotator cuff muscles, the head of the humerus (ball of the socket) will move too much and not stay in the socket. The rotator cuff muscles need to work in good synchronization, with supportive ligaments for full shoulder function. Furthermore, the glenohumeral joint flares easily. Treatment that pushes into pain will aggravate the condition.
A full subjective and objective assessment, of a ‘problem shoulder’, can take time. Therefore trying to diagnose in a normal consultation can raise difficulties.
When diagnosing soft tissue injuries of the shoulder it is wise to try to classify into 3 main subdivisions:
1. Impingement/Rotator Cuff injuries (more commonly seen)
2. Laxity/dislocation injuries.
3. Capsular Tendinitis/Frozen Shoulder
It may be necessary to rule out a host of differential diagnoses such as referred pain, bone involvement, spinal involvement, sporting technique/biomechanics etc, which can confuse the matter. Experience in orthopaedic shoulder tests is helpful. Looking at basic abduction, rotation, posture, the movement of the scapulae and impingement and stability tests should help to classify your patient.
As the shoulder joint is, in essence, a soft tissue joint, research shows the majority of problem shoulders will settle with exercise, modified rest and re-education. Anti-inflammatory medications are often beneficial in the acute stage. Further investigations such as X-ray and ultrasound are often needed to rule out tendon tears and degenerative change.
ROTATOR CUFF INJURIES
Rotator Cuff Injuries to the shoulder are common in all age groups. In the younger age group, they are usually acute and related to trauma, while in the older age group they are degenerative and often chronic. In this scenario, we will concentrate on the older degenerative rotator cuff.
As the shoulder joint is, for all accounts, a muscular joint, osteoarthritis is not commonly seen as in other joints. Rather the rotator cuff muscles, in particular, the supraspinatus tendon starts to fray. The subacromial bursa may become inflamed and the Acromion may develop spurs. The shape of the acromion itself may exacerbate these types of problems. In these patients, the thoracic spine is usually tight to compensate for the unstable rotator cuff. The scapular develops an abnormal rhythm over time and the patient will complain of upper arm pain. A painful Arc in abduction is common.
When assessing the suspected rotator cuff shoulder there are many tests but 2 important tests should be included. The first is an impingement test, such as Hawkins and Kennedy’s where the patient’s arm is placed in horizontal adduction and then internally rotated. Reproduction of the patient’s pain as end range adduction is reached is a positive test.
The second test is the empty can test, where the patient’s arm is placed in horizontal abduction in the line of the scapula (approximately 15 degrees forward of abduction). The thumb should point down and resistance is applied downwards. The patient must push up to maintain a static position. Pain should be noted but a weakness is more important as it may suggest a full or partial tear of the supraspinatus tendon.
Assessment should also include cervical and thoracic range/restriction, posture, scapular rhythm, rotation (passive, active and resisted), shoulder range in general and of course elimination of instability, frozen shoulder or differential diagnoses.
Ultrasound is the ideal test for diagnosis of rotator cuff injuries. Conservative treatment concentrating on exercise and posture is usually the first option for the older patient, and even full thickness tear patients often do extremely well. However, the unsuccessful conservative patients usually end up in surgery which has a high success rate despite a long rehabilitation period. Early passive mobilisation with physiotherapy is advised in the first 6 weeks of rehabilitation to avoid frozen shoulder complications and increase the chances of success.
THE UNSTABLE SHOULDER
Instability of the shoulder is commonly seen in association with other injuries such as rotator cuff, labrum tears, fracture, axillary nerve involvement, to name a few. It can occur in a traumatic situation, or over a period of time and this is when it can be more difficult to diagnose. Stretching of the shoulder capsule and the ligaments that are associated with it (anterior, medial and inferior) create the majority of the instability.
There are 3 main forms of instability:
1. Anterior (most commonly seen and often traumatic)
2. Posterior
3. Inferior (usually indicative of multidirectional laxness)
Anterior dislocations or subluxations occur usually when the arm is up at 90 degrees abduction and there is an anterior force from the back of the shoulder. The Apprehension test mimics this position and can be tested with the patient in sitting. Always compare both shoulders to get a feel of the normal shoulder movement of that patient.
Posterior dislocation is most likely to occur with the arm in flexion and the head of the humerus is forced back posteriorly. It is not commonly seen. This can be tested with the patient’s arm at 90 degrees flexion and applying a posterior pressure through the arm to the shoulder joint.
Inferior instability is most easily tested with the sulcus test of comparing the humeral head levels in the resting shoulder. Shoulders that dislocate or sublux on a regular basis will develop this instability and very occasionally it is seen in an acute instance from a caudal force to the shoulder.
Multidirectional instability usually occurs over a period of time although it can be initiated with a traumatic event. It is often treated with rehabilitation. Unilateral dislocations more commonly occur with trauma. Most Orthopaedic surgeons will stipulate the importance of surgery at an early stage to avoid further dislocation. This is especially important for the younger patient.
Instability in shoulders that are treated conservatively has a moderate success rate. Treatment usually concentrates on specific strengthening exercises and recent research shows that upper trapezius training and scapular stabilizing work may play a significant role in assisting to stabilise the unstable shoulder. Treatment usually results in some increased stability although, for the more aggressive sports, taping is recommended to avoid further damage. In some cases, surgery may be the only option.